
- Home
- Advice Hub
- Pregnancy
- Labour & Birth
- Induction Of Labour: What To Expect
Induction of Labour
Our experts explain essential information on induction of labour, including reasons, methods, and what to expect during the process.
The journey from pregnancy to birth is like no other. It is a rollercoaster of emotions from excitement to trepidation and ending with a moment of ultimate human connection.
While many pregnancies progress naturally to spontaneous labour between 37 and 42 weeks, there are many reasons why the labour may need to be started artificially. Predominantly, it's for the safety of the mother and the baby, this is called induction of labour (IOL).
What is Induction of Labour?
The National Institute of Health and Care Excellence (NICE) defines Induction of labour as: ”an intervention designed to artificially initiate uterine contractions leading to progressive dilatation and effacement of the cervix and birth of the baby”
Why Might Labour be Induced?
The decision to induce labour will be based on your unique set of circumstances. It is guided by clinical guidance, and a thorough discussion of the risks versus benefits between you and your obstetric team. The decision to proceed with, or decline, an induction of labour will ultimately be yours.
There are several clinical reasons why an induction of labour might be recommended. Decisions to induce labour are usually based on concerns around the health of the mother or the baby, if the pregnancy were allowed to continue.
The most common reason to be offered an induction of labour is for a pregnancy that reaches or passes 41 weeks gestation. This is also known as a prolonged pregnancy.
NICE recommends offering an induction of labour to expectant mothers with a prolonged pregnancy, as any pregnancy that extends beyond this carries an increased risk of stillbirth.
If you decide to decline the offer of induction of labour, your obstetric team will offer you increased monitoring of your baby’s wellbeing.
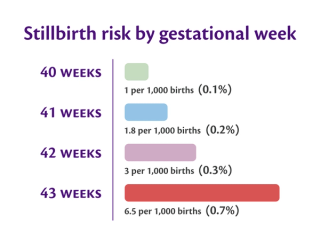
(Source: NICE Guideline NG207, RCOG)
Other key reasons include:
- Maternal health conditions, such as: gestational diabetes, pre-existing diabetes, high blood pressure, pre-eclampsia, or obstetric cholestasis of pregnancy.
- Prelabour Rupture of Membranes (PROM), this is when the waters break without contractions starting
- Fetal health conditions, such as: fetal growth restriction, reduced fetal movements or a suspected big baby.
Methods of Induction
There are several methods involved in the induction of labour process, steps are taken to soften/ripen the cervix (neck of the womb). Once achieved, the next stage is to initiate contractions.
Membrane sweep
The first step of an induction of labour is usually a membrane sweep. It can be performed from 39 weeks gestation and can be done in the home setting or in an antenatal clinic. There are no medications required.
A vaginal examination is performed by a midwife or doctor, during which they will sweep a finger around the inside of your cervix, separating it from the membranes surrounding your baby. This action helps your body to release its natural prostaglandins (hormones) which will encourage the cervix to soften and hopefully help kick start labour within 48 hours.
The membrane sweep can feel a little uncomfortable and focusing on deep slow breaths can help you to relax during the examination. You may notice some light spotting or bleeding which is accompanied by period-like cramps afterwards. This is normal and nothing to be worried about.
If the initial membrane sweep is unsuccessful in getting your labour to start, it can be repeated at 48-hour intervals and attempted up to 3 times. There are no known risks to having a membrane sweep.
Prostaglandin gel or pessary
If the membrane sweep has been unsuccessful and your cervix is not soft/ripe enough, you will be offered pharmacological methods to help ripen/soften your cervix.
A vaginal examination is performed by a midwife or doctor, during which a medication such as a prostaglandin gel, tablet or pessary (a synthetic version of your own hormone prostaglandin) is placed in the posterior fornix (an area high up and at the back) of the vagina. This medication will help soften/ ripen your cervix in preparation for labour.
Artificial rupture of membranes (ARM)
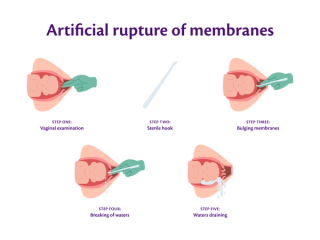
Your cervix is considered ‘favourable’ or ready when it has softened sufficiently and dilated a couple of centimetres. Once this has been achieved the next step is to break the waters. This is known as Artificial Rupture of Membranes (ARM) in medical terms.
To do this, a vaginal examination is performed by a midwife or doctor, during which they guide a sterile plastic hook, known as an amnihook, through the vagina and into the open cervix.
They will use their fingers to feel for the bulging sac of membranes surrounding the baby and gently tear a hole in it, allowing the waters to drain away. This release of water can be all that's required to get contractions going. Getting up and going for a walk after this procedure will help your baby's head move down into the pelvis and press down on the cervix which will further increase the likelihood of contractions starting.
Oxytocin infusion
Should contractions fail to start or are not considered to be strong enough following the rupture of membranes, the administration of an intravenous oxytocin infusion is usually required.
The oxytocin infusion uses a synthetic, more potent, and more powerful version of the naturally occurring hormone, oxytocin. It is administered via a drip in your arm, starting at a very low dose and increasing gradually until your contractions are strong enough and regular enough to support labour. Once the oxytocin infusion has been commenced your baby's heartbeat will need to be continuously monitored.
What to Expect During Induction
Close and consistent monitoring of both you and your baby is required throughout the process of labour induction. An induction of labour is a high risk procedure and must be conducted in a hospital setting.
Induction of labour can be a lengthy process. It often takes between twenty-four and forty-eight hours just to reach established labour.
It is important to understand that induced labour encourages your body to start before it is naturally ready, and often at a much faster pace than spontaneous labour. As a result, it can often feel more intense and more painful than if labour had started spontaneously.
It's crucial to discuss your options and preferences around pain relief with your midwife and obstetric team, ensuring your birth plan clearly documents and reflects your wishes.
Induction of labour can be associated with higher rates of medical intervention such as:
- Continuous fetal heart monitoring
- Requiring intravenous access for fluids (drips)
- More frequent vaginal examination to check the progress of labour
- A higher risk of requiring an instrumental delivery (assisted vaginal delivery with a forceps or kiwi).
The use of prostaglandins and oxytocin increases the risk of uterine hyperstimulation (contractions that occur one after another with no break in between), which can cause the baby's heart rate to drop and increase the risk of uterine rupture (tear in the wall of the uterus/womb).
Preparing for Induction
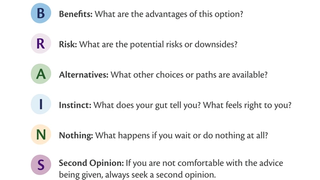
Being prepared for your induction of labour will help you feel empowered and in control. It's vital to discuss your options and preferences around the induction process with your obstetrician and midwife, and document these clearly in a birth plan. Using the BRAINs acronym can be really useful when making an informed decision:
B - What are the benefits?
R - What are the risks?
A - What are the alternative options?
I - What does my gut instinct tell me?
N - What happens if I do nothing?
S - Do I want a second opinion?
Having your hospital bags packed, childcare arranged (if you already have children) can be done weeks in advance of being admitted to hospital for your induction and you will feel great for having it ticked off your list of things to do.
Make sure to pack things like books, crosswords and download documentaries, films or podcasts to keep you occupied during your hospital stay, as induction of labour can be a long and drawn out process.
Conclusion
Induction of labour is a routine and safe procedure performed daily in hospitals. They are carried out by highly experienced doctors and midwives, adhering strictly to clinical guidelines, ensuring the safety of both the mother and the baby.
While it can be daunting having a medical intervention that interferes with the natural birth process, understanding what it involves and being a part of the decision-making process can help you to feel empowered and in control as you prepare to meet your baby.
FAQs around labour induction
Yes, when induction of labour is clinically justified, it is deemed safe and is performed to avoid complications which might occur if the pregnancy were allowed to continue.
There are risks associated with induction of labour such as a higher rate of instrumental delivery, increased risk of hyperstimulation or uterine rupture. However, it's important to know that midwives and doctors are highly trained to manage these situations should they occur, keeping both you and your baby safe.
A pregnancy sweep, or membrane sweep, is when a midwife or doctor performs a vaginal examination and separates the membranes from the bag of water around the baby away from the cervix. This causes the natural prostaglandins to be released. The goal is to encourage the onset of contractions and potentially avoid the need for any further pharmacological methods of induction.
Induction of labour can be more intense and painful than spontaneous labour due to its rapid onset. Everyone has a different pain threshold, and it can be difficult to know in advance how you will cope on the day. The best approach is to familiarise yourself with all the different pain relief options so you can confidently decide what you want on the day.
A water birth remains an option following a membrane sweep. However, if your labour induction involves an oxytocin infusion, continuous monitoring of your baby's heart rate will be necessary, which means a water birth will not be possible. It's always good to speak with your obstetric team, who can provide advice tailored to your specific circumstances.
Induction of labour is not always successful. If this happens, your obstetric team will reassess both you and your baby’s wellbeing. They may suggest taking a rest before trying again or they may schedule you in for an elective (planned) caesarean section.
