
- Home
- Advice Hub
- Pregnancy
- Pregnancy Symptoms & Issues
- Breech Baby: What It Means
Breech Baby: what it means and what to expect
Learn what a breech baby is, why it happens, how to encourage turning, and your options for a safe delivery if baby stays breech near term.
What is a breech baby?
When and why babies are breech
Types of breech positions
How breech babies are diagnosed
Can a breech baby turn on its own?
How to encourage your breech baby to turn
External cephalic version (ECV)
Delivery options for breech babies
Is a breech baby more painful to carry?
Long-term outcomes for breech babies
Can breech position be prevented?
Talking to your provider about breech
FAQs around the breech position
When a baby presents with their feet or bottom first this is known as breech presentation.
The ideal presentation is when the baby presents with their head down, which is called vertex presentation.
It is very normal for a baby to be breech during the early part of pregnancy, however, most have turned head down by 37 weeks. The percentage of babies’ breech at term is around 3-4%1.
This blog post provides information about what a breech baby is, why it happens, how to encourage turning, and your options for a safe delivery if the baby stays breech near term.
What is a breech baby?
A breech baby is one whose bottom, feet, or knees are positioned to come out first during birth, rather than the top of the head. The reason this position matters or could potentially be a cause for concern is that the baby's head is the largest part of the body. When the baby is head down, the head is the first part to dilate the cervix and pass through the birth canal, allowing for the rest of the body to follow easily. In a breech presentation, the baby's legs and buttocks are the first part to dilate the cervix and pass through the birth canal. The concern is that the cervix may not be dilated enough for the head to pass through and may get momentarily stuck.
When and why babies are breech
The majority of babies will turn their heads down by themselves between 32 and 36 weeks of pregnancy. After 36 weeks, the chances of a baby turning naturally decreases due to the lack of space in the uterus.
We don't always know why some babies present bottom or feet first, however there are certain factors which can contribute to a baby remaining persistently breech after 36 or 37 weeks of pregnancy. These include:
Uterine Shape/Structure: The presence of fibroids or an unusually shaped uterus can limit the amount of space a baby has to move about.
Amniotic Fluid Levels: If there is too much fluid in the uterus (polyhydramnios) this can make it difficult for the baby to adopt a stable head down position, equally if there is too little fluid (oligohydramnios)this can make it difficult for the baby to turn into a head down position.
Placenta Previa: This is when the placenta partially or completely covers the opening of the cervix. If the cervix completely covers the opening of the cervix, this can prevent the baby's head from engaging in a head down position.
Multiple Pregnancies: When there is a twin/multiple pregnancy, space within the uterus is limited and the odds of one or more of the babies presenting as breech is increased.
Types of breech positions
Understanding the specific type of breech can influence delivery decisions. The main types include:
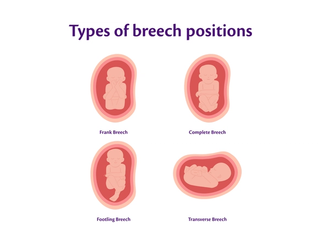
| Breech type | Description |
|---|---|
| Frank Breech | The baby's bottom is down, their legs are folded straight up at the hips, with their feet up by their head. |
| Complete Breech | The baby is in a sitting position with their bottom down and both knees bent, with their feet tucked close to their bottom . |
| Footling Breech | One or both of the baby’s feet are positioned below their bottom. |
| Transverse Lie | The baby is lying horizontally across the abdomen, not head down or bottom down. |
How breech babies are diagnosed
As part of your antenatal check-ups, your midwife or doctor will routinely check the baby's position.
Your midwife or doctor will assess the baby’s presentation from about 36 weeks onwards, they will do this by palpating your abdomen to determine which part of the baby is presenting. If the baby is head down, the round hard head is very easy to identify. If it's the baby’s bottom or legs which are presenting, they will feel softer, and more irregular.
An ultrasound scan is always performed whenever a breech presentation is suspected. It will confirm the baby’s exact position, placental location and volume of amniotic fluid. Most breech presentations are diagnosed between 32 and 36 weeks. While most babies have turned head down by this time, a small number can still flip spontaneously up to about 37 weeks.
Can a breech baby turn on its own?
Yes, most breech babies turn head down by themselves!
Before 36 weeks: The odds of the baby being able to turn naturally is quite high due to the fact that it still has plenty of space to do so.
After 37 weeks: Whilst it's not impossible, the odds of the baby being able to turn head down spontaneously after 37 weeks is quite low due to the baby’s size and the now limited space within the uterus.
Early Labour: While it's not very common, some babies may turn head down in the very early stages of labour. I have seen this happen a handful of times over the last 30 years.
How to encourage your breech baby to turn
If a baby is breech late in pregnancy (37 weeks or more), some people try the following natural methods to encourage the baby to move. It is really important to speak with your midwife or doctor first if you are planning to try these. There isn't much evidence to support them, but they are generally safe to try:
Breech Tilt/Bridge: Laying on your back with your hips raised above your shoulders supported by pillows, the idea is that this position will help your baby's bottom to shift out of the pelvis.
Inversion Poses: Yoga positions such as the Child’s Pose or leaning forward on hands and knees, can help by using gravity to create more space in the lower pelvis allowing the baby's bottom to move freely.
Temperature or Sound: Playing music towards the bottom of your abdomen might encourage your baby to move towards the sound. Placing a bag of cold peas near the top of the uterus may encourage your baby to move away from the cold.
Acupuncture/Moxibustion: Some people try these complementary therapies, but there isn't much evidence to support them.
External cephalic version (ECV)
If you reach 36-37 weeks of pregnancy and your baby is still breech, your doctor may talk to you about the possibility of doing an External Cephalic Version (ECV).
An External Cephalic Version involves a procedure which attempts to physically turn the baby from a breech position to a head down position. The doctor applies a firm but gentle pressure to your abdomen to do this. It is always carried out in the hospital setting and is done around 37 weeks of pregnancy. The ECV is performed using ultrasound guidance (to visualise baby’s position) and the baby’s heart rate is monitored throughout. To increase the chance of it being successful, a medication called a tocolytic (prevents the uterus from contracting) is given before the procedure is carried out.
ECV are successful in about 50% of cases2. However, it does come with some potential risks which are rare. These include causing the baby’s heart rate to drop or labour being triggered. Both of these risks are rare. If you have certain complications such as a low lying placenta, it will not be offered as an option to you.
Delivery options for breech babies
If a baby is still breech after 37 weeks and ECV is not an option or has not been successful, your obstetrician will discuss other options available to you. The decision will factor in your preferences, your medical history, the type of breech, and the level of expertise of your obstetric team.
Planned C-section for breech position
The most common recommendation is being offered an elective (planned) Caesarean section (C-section) for the birth of a breech term baby. An elective Caesarean section is normally performed around 39 weeks . It involves a surgical incision in the abdomen through which the baby is delivered. The National Institute of Care and Health Excellence (NICE) states that an elective C-section is the safest option for the delivery of a breech baby.
Vaginal breech birth
Some people opt for a vaginal birth with the support of an obstetrician or midwife who have extensive experience in delivering breech term babies. A planned vaginal breech birth is considered more favourable if you have previously had a vaginal birth, the baby is a good size, and the pelvis is adequate.
It requires a hospital with staff experienced in this specialised method and continuous fetal monitoring. The main benefit of a vaginal breech birth is that it avoids abdominal surgery and its associated risks for the mum. However, the risk of complications to the baby are higher in comparison to having an elective C-Section. A vaginal breech birth may not be an option as planned term breech deliveries become less and less common, there are now less, and less Midwives and Doctors trained to support them.
Emergency breech delivery
In situations where the baby's breech presentation is unexpectedly discovered in advanced labour, the obstetric team (doctors and midwives) will need to make a speedy decision about the delivery. This may involve proceeding with a vaginal delivery, under the specific circumstances mentioned above, or to go ahead with a category 1 (emergency) caesarean section.
Discovering a baby being breech this late is very rare, however the obstetric team attend regular training sessions and are therefore well rehearsed on how to manage unexpected and undiagnosed breech presentations.
Is a breech baby more painful to carry?
A breech presentation should not cause you pain. However, due to the positioning of the baby’s head and legs you may well feel discomfort from the hardness of the head or kicking of the legs around your rib cage.
Long-term outcomes for breech babies
The majority of babies who are born breech, whether by Caesarean section birth or vaginal birth go on to live perfectly healthy lives.
The primary concern which is unique to breech presentation is the development of the hips, especially if the baby was in the frank breech position for a considerable amount of time.There is a marginally higher risk of Developmental Dysplasia of the Hip (DDH), (an instability of the hip joint), with breech presentation.
Every baby has the NIPE exam (Newborn and Infant Physical Examination) within 72 hours of the birth. This can be carried out by a paediatrician or specially trained midwives. Part of this exam is to assess for DDH.
Any baby that was breech at 36 weeks of pregnancy is also offered an ultrasound of the hips as standard in the UK at 6 weeks old to check for DDH. This allows for timely detection and treatment if required.
Can breech position be prevented?
The position of a baby, whether breech or not, is largely beyond a person's control. Factors that determine the baby's position such as placental location, the shape of the uterus, the orientation of the pelvis, and the volume of amniotic fluid are unchangeable.
The focus should be on raising awareness and making the appropriate preparations for birth, rather than attempting to prevent a breech position.
Talking to your provider about breech
If you are told your baby is breech at term, it is vital to have open discussions with your midwife or doctor. Shared decision making is crucial.
Key questions you may want to ask include:
"Can you explain the type of breech position my baby is in” and "what are the implications for delivery?"
"Do I meet the criteria for an External Cephalic Version (ECV)?"
"How many ECV’s have you performed?” What is your success rate”?
"What are the hospital's policies and success rates for planned vaginal breech birth?"
"If I choose to have a vaginal breech birth outside of hospital guidelines, will I be supported?"
It is completely understandable to be worried if you are near your due date and your baby is breech. However, please be assured that there are lots of safe options available to you for the birth. It really depends on the baby’s position and your overall health. A safe outcome for both you and your baby is always the goal.
FAQs around the breech position
Breech presentation is incredibly common in the second trimester and is not considered to be an issue early on. Breech presentation only becomes a concern if it persists beyond 36 weeks of pregnancy and this is because of the potential complications it can pose for delivery. All obstetric teams are highly skilled in managing breech births safely whether that by caesarean section delivery or vaginal breech delivery under specific circumstances.
Most babies naturally turn head down by 36 weeks of pregnancy.
While some may turn later, turning becomes less likely after 37 weeks due to the baby’s size and lack of space in the uterus.
Persistent breech presentation can be due to factors such as lack of space in the uterus, the shape of the uterus, the location of the placenta or the amount of amniotic fluid (too much or too little). Sometimes there is no obvious reason for why a baby has remained in the breech position.
Starting labour with a breech baby is the same as with a head down baby, with the onset of contractions or your water breaking.
There are lots of things you can try to help turn your breech such as :
- Specific yoga positions like the breech tilt or all fours position
- Applying sound and cold to the abdomen
- Complementary therapies like acupuncture and chiropractic care
Always speak with your midwife or doctor before attempting any of these techniques.
