
- Home
- Advice Hub
- Pregnancy
- Pregnancy Symptoms & Issues
- What Is An Ectopic Pregnancy?
What is an Ectopic Pregnancy?
Learn about causes, symptoms, diagnosis, treatment, and fertility options in this expert-led pregnancy guide.
How common is ectopic pregnancy?
When to seek medical help
How an ectopic pregnancy is diagnosed
Treatment options and what to expect
What causes an ectopic pregnancy?
Can ectopic pregnancy be prevented?
Will I be able to get pregnant again?
Fertility options after ectopic pregnancy
Follow-up care after ectopic pregnancy
Emotional impact and support after loss
FAQs around ectopic pregnancy
An ectopic pregnancy is where a fertilised egg implants outside the womb. In most ectopic pregnancies, the fertilised egg implants in one of the fallopian tubes. Less commonly, the fertilised egg implants in the ovary, cervix, or abdomen. It can also implant in a caesarean scar, or other places within the womb wall. Even though it’s in the wrong place, the egg will still try to develop and get bigger. As it gets bigger, an ectopic pregnancy can rupture (burst), this can be life threatening. Unfortunately it is not possible to save the pregnancy, and usually has to be removed using medicine or an operation.
More information on this can be found on NHS .
How common is ectopic pregnancy?
While uncommon, ectopic pregnancies aren't rare, affecting about 1 in 90 pregnancies in the UK. This means approximately 11,000 cases are diagnosed annually. While anyone can have an ectopic pregnancy, certain factors can increase the risk, such as having a history of pelvic inflammatory disease or previous ectopic pregnancies.
Early signs and symptoms to look out for
It's crucial to be aware of the signs and symptoms of ectopic pregnancy, as early detection is vital for a safe outcome.
Early warning signs
The earliest signs of ectopic pregnancy can be subtle and easily confused with a normal pregnancy or other conditions. Ectopic pregnancy symptoms include:
- A missed period.
- Light vaginal bleeding or spotting that is different from your usual period.
- Mild pain in your lower abdomen, which may feel sharp, dull, or crampy, and is often localised to one side.
For more information on what to expect in the early stages of pregnancy, see our guide on the first trimester.
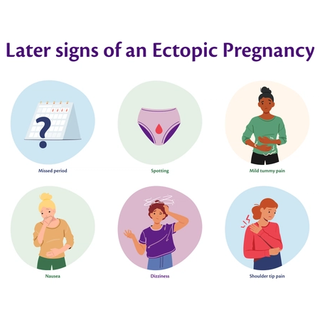
Later or more serious symptoms
As an ectopic pregnancy progresses, more urgent symptoms can develop. These indicate a more serious condition and require immediate medical attention:
- Sudden, severe abdominal pain.
- Shoulder tip pain, which is a sharp pain at the tip of the shoulder. This is caused by internal bleeding irritating a nerve under the diaphragm.
- Dizziness or fainting due to a drop in blood pressure from internal bleeding.
- Nausea, diarrhea, or vomiting.
If you experience these symptoms, it's essential to seek medical help immediately.
When to seek medical help
Knowing when to act is vital. Always trust your instincts if something doesn't feel right.
When to contact your GP or 111
If you have any of the early warning signs mentioned above and suspect you might be pregnant (even with a negative test), contact your GP or call NHS 111 for advice. They can help you determine the next steps and get a proper diagnosis.
When to call emergency services
If you experience any of the serious or escalating symptoms, such as sudden, sharp abdominal or shoulder tip pain, fainting, or collapse, call 999 or go to the nearest A&E immediately. An ectopic pregnancy can cause life threatening internal bleeding if the fallopian tube ruptures, so acting fast is crucial.
How an ectopic pregnancy is diagnosed
If an ectopic pregnancy is suspected, you'll be referred to an early pregnancy assessment unit (EPAU) for a diagnosis. The process usually involves:
- Pregnancy tests: A urine or blood test to confirm pregnancy.
- Ultrasound scan: A transvaginal ultrasound is used to look for the pregnancy sac inside the womb. If nothing is seen, an ectopic pregnancy is suspected.
- Blood tests: Your hCG (human chorionic gonadotropin) levels may be monitored over 48 hours to see if they are rising as expected. In a healthy pregnancy, these levels double every 48–72 hours; in an ectopic pregnancy, they often rise more slowly.
Treatment options and what to expect
Once diagnosed, the treatment depends on the size of the ectopic pregnancy, your symptoms, and your hCG levels. The three main options are:
- Expectant management: If the pregnancy is very small and your hCG levels are low and falling, doctors may opt for a "wait and see" approach. You'll be closely monitored with blood tests and scans to ensure the pregnancy resolves on its own. The aim is to let the body end the pregnancy, without any medical intervention.
- Methotrexate: For some, methotrexate, a medication that stops the pregnancy from growing, is used. This is a non surgical option that allows the body to absorb the tissue over time.
- Laparoscopy (surgery): If the ectopic pregnancy is larger or causing symptoms, surgery is often necessary. A keyhole surgery called a laparoscopy is performed to remove the ectopic pregnancy, and sometimes the fallopian tube is removed as well.
What causes an ectopic pregnancy?
While the cause is sometimes unknown, an ectopic pregnancy is more likely to occur if you have the following risk factors:
- Previous ectopic pregnancy
- Fertility Treatment - An ectopic pregnancy can occur during IVF treatment as embryos can travel into the fallopian tube during the implantation stage. The more embryos transferred the higher the risk.
- Older age (35 years or above).
- Pelvic Inflammatory Disease (PID), often caused by sexually transmitted infections (STIs) like chlamydia. PID can cause scarring and blockage of the fallopian tubes increasing the risk of an ectopic pregnancy.
- Damage to the fallopian tubes, often from a previous infection, surgery, or endometriosis.
- Endometriosis - it is not known why this increases the risk of an ectopic pregnancy
- Abdominal Surgery - abdominal surgery can cause scar tissue and adhesions which can block or damage the fallopian tubes, increasing the risk of an ectopic pregnancy.
- Contraceptive Intrauterine Devices - (IUD’S) are very good at preventing pregnancy in the womb but not in the fallopian tubes.
- Emergency contraception - if emergency contraception fails to prevent ovulation the risk of ectopic pregnancy is increased.
- Cigarette Smoking - smokers have an increased level of PROKR1 in their fallopian tubes, this can hinder the progress of a fertilised egg, increasing the chances of an ectopic pregnancy.
You can get more support at the Ectopic Pregnancy Trust.
Can ectopic pregnancy be prevented?
It's not always possible to prevent an ectopic pregnancy, but you can reduce your risk by making healthy lifestyle choices, such as quitting smoking, and protecting yourself from STIs by using condoms. Regular sexual health checks are also a good idea.
Will I be able to get pregnant again?
For many people, the answer is yes. Going on to have a healthy pregnancy after an ectopic pregnancy is very common. The chances of a successful pregnancy depend on whether the fallopian tube was removed and the condition of the remaining tube. Many people conceive naturally, but if you have both tubes blocked or removed, you may need to consider other fertility options. It is generally recommended to wait at least two menstrual cycles after treatment before trying to conceive again.
Fertility options after ectopic pregnancy
If you find that your fertility has been affected, don't lose hope. Many people can still conceive naturally. If not, your GP or a fertility specialist can discuss options like IVF, which can help you conceive by bypassing the fallopian tubes.
Follow-up care after ectopic pregnancy
After treatment, you'll need follow-up care to ensure a full recovery. This may include:
- Blood tests to monitor your hCG levels until they return to zero.
- Rest and emotional recovery. It's important to give your body and mind time to heal.
- Follow-up appointments with your doctor to discuss your recovery and future pregnancy plans.
Emotional impact and support after loss
An ectopic pregnancy is a significant loss, and it's completely normal to feel a range of emotions, including grief, sadness, anger, or anxiety. It's a loss that isn't always recognised or talked about, which can make it even more difficult.
- Seek support: Don't feel you have to go through this alone. Reach out to a partner, family, friends, or a therapist.
- Consider professional help: Organisations like The Ectopic Pregnancy Trust offer excellent resources, support groups, and a helpline to connect with others who understand what you're going through.
- Validate your feelings: Allow yourself time to grieve and process the loss.
For more support and information on dealing with pregnancy loss, you can read our guide on miscarriages .
FAQs around ectopic pregnancy
Ectopic pregnancies are most often caused by issues with the fallopian tubes, such as scarring or blockage, which prevent the fertilised egg from reaching the womb. However, sometimes the cause is unknown.
While both result in the loss of a pregnancy, they are not the same. A miscarriage is the loss of a pregnancy that has implanted in the womb. An ectopic pregnancy occurs when the embryo implants outside the womb and can't develop, and it poses a serious risk to the mother's health.
Three common signs are:
- Light vaginal bleeding or spotting.
- One-sided pain in the lower abdomen.
- Shoulder tip pain, which is a red flag for internal bleeding.
An ectopic pregnancy usually becomes apparent between 4 and 12 weeks of pregnancy. It cannot continue and must be treated to prevent life threatening complications. The length of time it lasts depends on the individual circumstances and how quickly it is diagnosed.












